Dry Eye Disease
What is Dry Eye?
Do your eyes burn? Do they feel like a piece of sand is in them or they will not stop watering? You are not alone. As of 2022, 16.8 million people have been diagnosed with dry eye. Most try to ignore it or self diagnose and do not get fully evaluated. It is a chronic condition where the eyes do not get the moisture needed to keep the cornea lubricated. Your tears are composed of three layers. Each layer is important for providing nutrition, protection, and comfort. A decrease in quality and/or quantity of any tear layer can lead to Dry Eye Disease (DED).

What are the symptoms?
Irritation, red eyes and/or eyelids, itching, burning, matted/sticky eyelids (especially in the morning), gritty eyes or foreign body sensation, sore/tired eyes, occasional or constant watery eyes, light sensitivity, fluctuating vision, decrease in contact lens wear/tolerance, styes or chalazions.
What causes Dry Eye Disease?
- Your own body’s oil quality and consistency plays a role. Those with dandruff or oily skin are more likely to have Blepharitis and Rosacea.
- Age: tear production normally decreases with age.
- Gender: women more likely than men due to changes in hormones and the use of oral contraceptives.
- Environmental factors: allergens, fans, heat and air conditioners, smoke, wind, very dry climates.
- Systemic conditions: Rosacea, Acne, Psoriasis, Rheumatoid arthritis, Sjorgen’s syndrome, Thyroid disease, Diabetes, Vitamin A deficiency, Lupus, Scleroderma and more.
- Bacteria and/or Demodex on the lid margin
- Certain medications: Retinoic acid (acne medicine), Hormone replacement therapy for menopausal women, Antihistamines (OTC allergy medicines, decongestants), Antidepressants, Anxiety, Diuretics (water pills), Beta blockers (for heart problems or blood pressure), Sleeping pills, Birth control, Prostate medications, Glaucoma medications and others.
- Contact lens wearers: overwear or wearing for many years.
- Ocular surgeries: cataract surgery and LASIK. After either of these, the corneal surface is compromised and untreated DED makes symptoms more evident.
- Gland damage from lack of blinking, inflammation or radiation.
- Prolonged reading and use of computers/video games/phones reduces blinking which leads to reduced meibomian gland usage.
Diagnosing Dry Eye Disease
If you think you are suffering from dry eye, we recommend getting a dry eye evaluation. This examination determines your risk of dry eye, tracks your symptoms, and uses specialized diagnostic equipment to evaluate your tear quality and quantity to determine your treatment options.
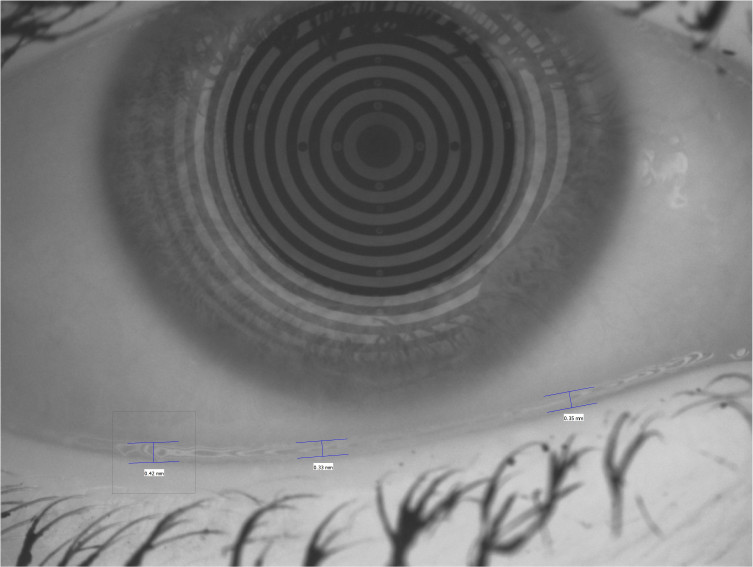
- Meibography is a diagnostic tool that images the oil glands in the eyelid to check for damage or loss
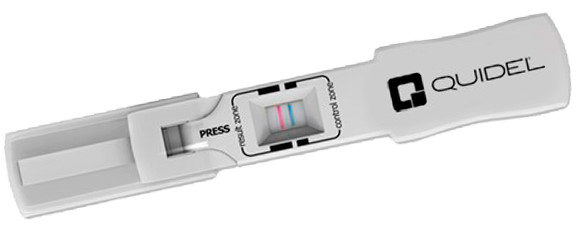
- Inflammation testing uses a diagnostic tool to collect a sample of tears which measures a molecule called MMP-9. This molecule causes inflammation in the tears. This test is imperative to choose the correct treatment for your dry eye.
- Tear testing measures your tear volume and evaporation rate of the tears.
- Slit lamp biomicroscopy with staining dyes evaluates the quantity of open Meibomian oil glands, checks the tear breakup time of the tear (how fast the tears evaporate), and checks for cornea damage using instillation of dyes.
How do I prepare for my dry eye evaluation?
- Do not wear contact lenses 2 hours prior to your visit
- Do not use any eye drops, OTC or medicated, 2 hours before your appointment
- Bring any drops you are currently using
Aqueous Deficient Dry Eye

What is Aqueous Deficient Dry eye?
When your eyes do not produce enough tears. The watery (aqueous) layer of the tear is produced by the lacrimal gland located in the upper outer corner of each eye. The aqueous layer of the tear is made up of water, vitamins, protein, electrolytes and other substances that help lubricate the eye, wash away debris and maintain a clear tear film.Treatment options:
- Artificial tears: Drops that lubricate and temporarily relieve symptoms. Available over the counter, but some contain lipids and oils which help prevent tear evaporation.
- Ointments: Thick lubrication used at night to cover the eyes while sleeping. Recommended for people with eyelids that do not close while sleeping, have sleep apnea, or have significant dry eye staining on examination.
- Omega Supplements: Omega 3 supplements in triglyceride form high in EPA, DHA and GLA are best absorbed by the body and have been shown to improve dry eye symptoms. Studies have found that fish oil and some over the counter omegas are found in ester form. Ester forms are not well absorbed by the body. They are produced in unpurified ethyl ester form and do not go through the process of re-esterification (a more costly process) which brings it back to the triglyceride form. Omegas found in our diet (flax seed/chia seed/seaweed/some nuts, etc) mostly contain ALA, which has a low conversion to DHA and EPA and cannot give our bodies the levels needed for systemic improvement.
- Punctal occlusion: A quick and painless procedure in which the doctor inserts a temporary or permanent plug into the lower and/or upper punctum. This reduces drainage and keeps the tears on the eyes longer.
- Immunosuppressive medications: Prescription drops which target inflammation in the lacrimal gland and tears.
- Prescription nasal sprays: A spray that activates the receptors in the nose which increases tear production.
- Serum Tears: Custom artificial tears made from serum, which is a component of your own blood.
- Amniotic Membranes: An FDA approved membrane made from avascular fetal cells. It promotes rapid corneal healing in severe cases only with corneal involvement.
- Scleral Contact lenses: Large hard contact lenses that cover the cornea and part of the sclera to keep the surface of the eye constantly lubricated when worn. Not offered at CFEC.
Evaporative Dry Eye/Meibomian Gland Dysfunction (MGD)
What is Evaporative Dry Eye?
Dry eye caused by the blockage or abnormality of the oil glands (meibomian glands) inside the eyelid. When the oil (meibum) cannot come out of the glands with a normal blink, the tear film has too much water and evaporates at a faster than normal rate. Chronic blockage causes inflammation and long term scarring that may lead to atrophy (loss) of the glands. Most people with dry eyes have some degree of MGD.Treatment options:
- Heat Compresses: Meibomian gland oil needs a specific temperature and duration to melt the meibum to help remove obstructions and thin the oil. Doctor approved microwavable, thermal and USB masks accomplish this.
- Artificial Tears: Drops with a lipid component to keep the tear from evaporating and keep them on the eye for a longer duration.
- Omega supplements: Omega 3 supplements in triglyceride form high in EPA, DHA and GLA are best absorbed by the body and have been shown to improve dry eye symptoms. Studies have found fish oil and some over the counter omegas are found in ester form. Ester forms are not well absorbed by the body. They are produced in unpurified ethyl ester form and do not go through the process of re-esterification (a more costly process) which brings it back to the triglyceride form. Omegas found in our diet (flax seed/chia seed/seaweed/some nuts, etc) mostly contain ALA, which has a low conversion to DHA and EPA and can not give our bodies the levels needed for systemic improvement.
- Prescription medications: Drops with a molecule with a similar composition to meibum. This drop keeps the tears from evaporating, keeping the tear film stable on the eye.
- Gland treatments: Manual or mechanical expression of the meibomian glands to unblock and remove any thick oils preventing the expression of thin meibum when you blink.

Lipiflow Thermal Pulsation System
What is it?
-12 min FDA approved treatment for meibomian gland dysfunction -Works by warming up the inside of the eyelids (where the meibomian glands are located) to remove blockages and restore healthy oil production, which will improve tear quality
What is involved in a procedure?
2. Anesthetic eye drops are instilled
3. Applicators are placed onto the eyelids
4. Treatment is started and takes 12 minutes. The process involves heat with rounds of gentle pressure to get the meibum (oil) to the perfect temperature to remove those blockages.
5. Applicators are removed and treatment is finished
What is the recovery time like?
There is no recovery time needed. Patients can return to normal activities immediately.
How long will it take to feel improvement?
Each patient has different levels of gland dysfunction, so each person will have different outcomes. Some will feel a difference immediately, others with significant gland dysfunction may take a few months.
What happens if I don’t get gland treatment?
Meibomian gland dysfunction is a chronic condition that will worsen over time. Without effective treatment, gland health will decrease, possibly leading to permanent loss of gland function, causing debilitating symptoms and a decrease in vision.Rosacea
What is Rosacea?
A chronic inflammatory condition that affects the face, eyelids and glands. A patient can have rosacea of the face (on the nose/cheeks/forehead) with or without having ocular rosacea and vice versa. It is important to diagnose and treat ocular rosacea in order to prevent permanent changes in the eyelids and damage to the meibomian glands.
What causes it?
The exact cause is unknown; it is thought to have both hereditary (genetic) and environmental components. It may be caused by swelling of the blood vessels of the skin in the affected areas. Some studies implicated an overgrowth of certain bacteria, which is why it is associated with a higher incidence of infections with blepharitis/demodex and styes (chalazion/hordeolum).
Symptoms:
Some patients may be asymptomatic, others may have chronic ocular irritation, redness, burning, watery eyes, light sensitivity, foreign body sensation, redness and swelling on the eyelids.Treatment options
- Warm compresses and eyelid scrubs if associated with Blepharitis/Demodex or MGD.
- Omega supplements: Naturally decrease inflammation from the source.
- Oral antibiotics: Used to decrease the bacterial load and inflammation of the soft tissues of the eyelids causing the swelling.
- Intense Pulsed Light (IPL): Controlled high intensity broad-spectrum light pulses to remove the superficial vessels by coagulating the capillaries which will reduce inflammation and eliminate facial redness. This requires between three and six treatments that are usually performed two weeks apart. As ocular rosacea is a chronic condition, retreatments may be required in the future to maintain improvement. Currently not offered at CFEC
Blepharitis

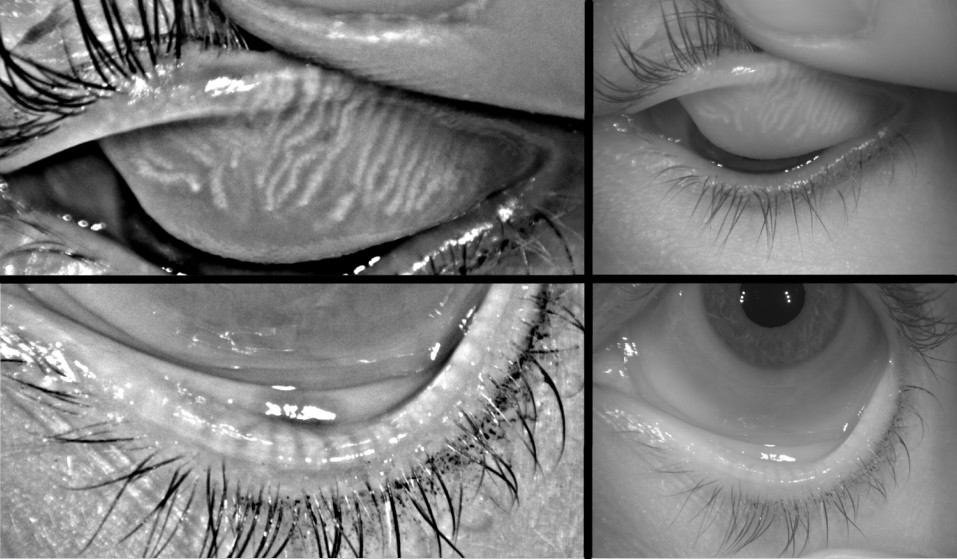
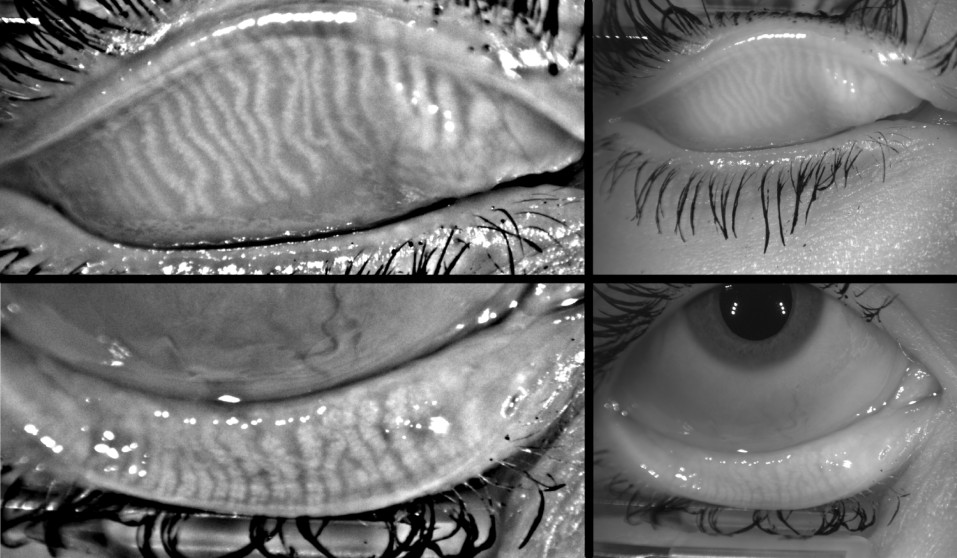
What is Blepharitis?
-Chronic inflammation and buildup of bacteria and debris on the eyelids. It can cause crusty dandruff-like flakes along the base of the lid margin. Can occur at any time and any age.
What is Demodex?
The most common extra parasite on humans, it is found on the skin, especially on the cheeks, nose and eyelids. Demodex is found on healthy, asymptomatic patients of all ages, but when at an increased level, it can lead to worsening symptoms.
Causes of Blepharitis/Demodex
Normal bacteria and Demodex live on our skin, this is to regulate our skin. The problem starts when there is too much bacteria or clogged oil glands which occur with dry eye, lack of blinking, allergies, dandruff, not removing makeup properly, certain medications or skin conditions such as Rosacea. Depending on the type of bacteria and quantity, the bacteria will build up on the lashes and demodex will increase and cause symptoms.
Symptoms of Blepharitis/Demodex
-Itching, redness on eyelids, lashes that stick together/get matted, swollen eyelid margins, burning and gritty sensation of the eyes, abnormal eyelash growth or a loss of lashes, recurrent styes or infections.Treatment:
- Lid scrubs: Over the counter as a spray, foam, gel or individually packaged towelettes, often containing hypochlorous acid, tea tree oil or okra based systems.
- Prescription options: Immunomodulators, Steroids, Anti-Bacteria and Antiparasitic medications are available depending on the type of blepharitis.
- In office eyelid exfoliation and debridement:
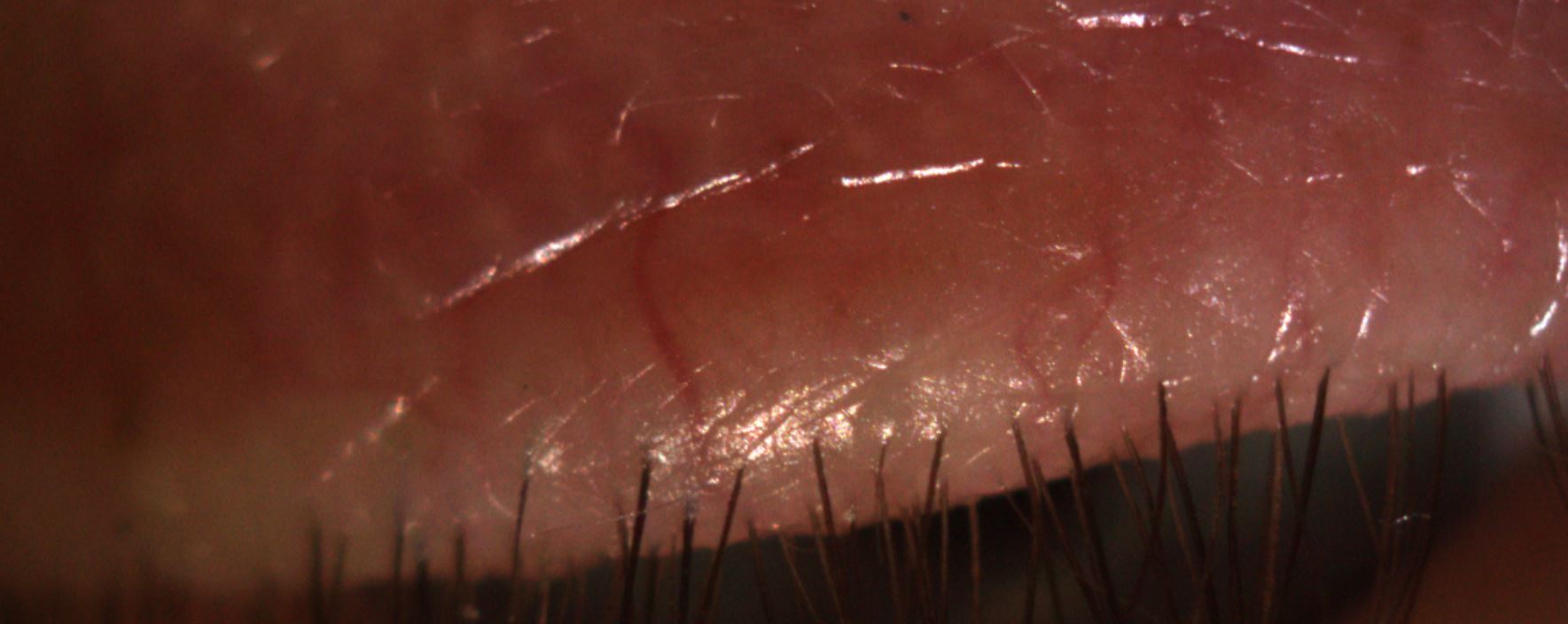
ZEST: Zocular Eyelid System Treatment: An exciting new treatment for the elimination of surface Demodex and Blepharitis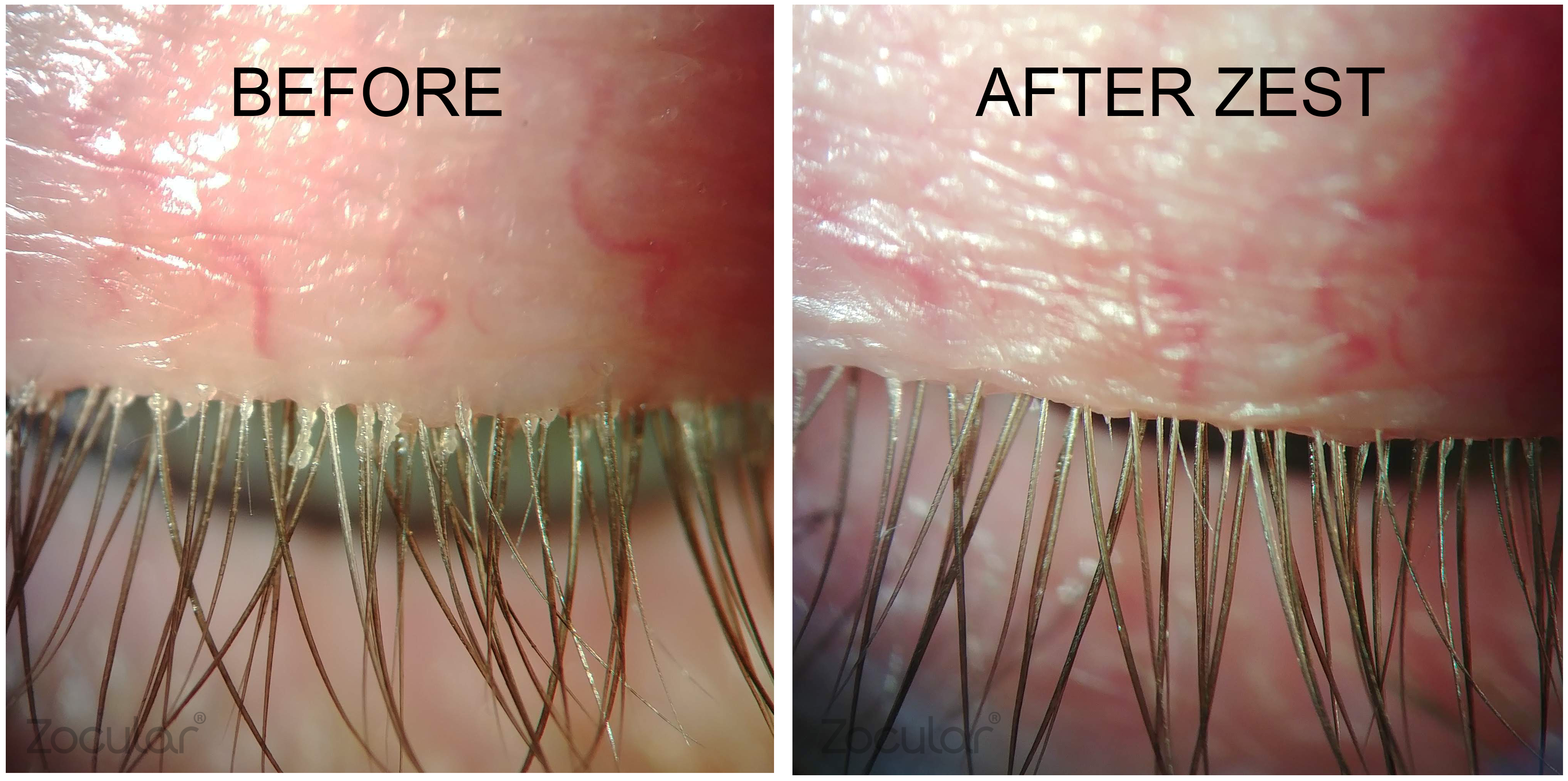
- Quick, painless, and brings immediate relief to the eyelids
- Formulated with refined extract of okra which removes debris and bacteria build up while soothing inflammation.
- After the procedure we recommend home treatments to keep the bacteria after demodex mites from returning.
- Works very well in combination with medications for full eradication of Demodex
- Done before gland treatments to remove the biofilm and bacteria from the glands
